Diabetes, a word commonly heard and often associated with sugar levels and insulin shots, is a condition that affects millions worldwide, but do you really know diabetes?
Do we truly comprehend the intricacies of this disease? Do we understand the profound impact it has on individuals, families, and societies at large? Beyond the conventional wisdom of “watch your sugar intake” lies a multifaceted condition that encompasses various types, each with its unique characteristics and challenges. From Type 1, an autoimmune condition where the body attacks its insulin-producing cells, to Type 2, often linked with lifestyle factors but increasingly recognised for its genetic components, diabetes manifests in diverse ways, defying simple categorisation.
But diabetes isn’t merely a matter of glucose regulation; it intertwines with numerous bodily systems, affecting everything from cardiovascular health to neurological functions. Its repercussions extend far beyond blood sugar fluctuations, influencing quality of life, lifespan, and even mental well-being.
Moreover, diabetes isn’t a solitary struggle; it reverberates through communities, economies, and healthcare systems. Its prevalence is on the rise, propelled by factors ranging from sedentary lifestyles to socioeconomic disparities. Understanding diabetes necessitates not only grasping its biological mechanisms but also acknowledging the social, economic, and cultural contexts in which it thrives.
According to Diabetes UK data shows that more 4.3 million people in the UK live with diabetes. Additionally, 850,000 people could be living with diabetes who are yet to be diagnosed. These registration figures for 2021-22 are up by 148,591 from 2020-2021.
Join us as we ask: Do you really know diabetes?
What is Diabetes
Diabetes is a chronic health condition characterised by elevated levels of glucose (sugar) in the blood. Glucose is the primary source of energy for the body’s cells, and its levels are regulated by insulin, a hormone produced by the pancreas. When someone has diabetes, their body either doesn’t produce enough insulin or doesn’t use insulin effectively, leading to high blood sugar levels, known as hyperglycaemia.
There are several types of diabetes, each with its own causes, symptoms, and treatments:
- Type 1 Diabetes: This type of diabetes is an autoimmune disease where the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. As a result, people with Type 1 diabetes require lifelong insulin therapy to regulate their blood sugar levels. Type 1 diabetes often develops in childhood or adolescence, although it can occur at any age.
- Type 2 Diabetes: Type 2 diabetes is the most common form of diabetes, accounting for the majority of cases worldwide. In Type 2 diabetes, the body becomes resistant to the effects of insulin or doesn’t produce enough insulin to maintain normal blood sugar levels. Risk factors for Type 2 diabetes include obesity, sedentary lifestyle, genetics, and age. Initially, lifestyle changes such as diet and exercise may be recommended, but some people with Type 2 diabetes may also require medication or insulin therapy.
- Gestational Diabetes: This type of diabetes occurs during pregnancy when the body is unable to produce enough insulin to meet the increased demand. Gestational diabetes typically resolves after childbirth, but women who develop it are at increased risk of developing Type 2 diabetes later in life.
- Other Forms of Diabetes: There are also other, less common forms of diabetes, such as monogenic diabetes (caused by mutations in a single gene) and secondary diabetes (resulting from other medical conditions or medications).
Uncontrolled diabetes can lead to serious complications, including cardiovascular disease, kidney disease, nerve damage (neuropathy), eye damage (retinopathy), and foot problems. Therefore, proper management of diabetes through medication, lifestyle modifications, regular monitoring of blood sugar levels, and ongoing medical care is essential in preventing or delaying these complications and maintaining overall health and well-being. We hope this helps to answer – do you really know diabetes.
What are the signs and Symptoms – do you really know diabetes
The signs and symptoms of diabetes can vary depending on the type of diabetes and the individual’s specific circumstances. Here are some common signs and symptoms to be aware of, to understand do you really know diabetes:
- Frequent Urination (Polyuria): Excess sugar in the blood can cause the kidneys to work harder to filter and absorb the glucose, leading to increased urination.
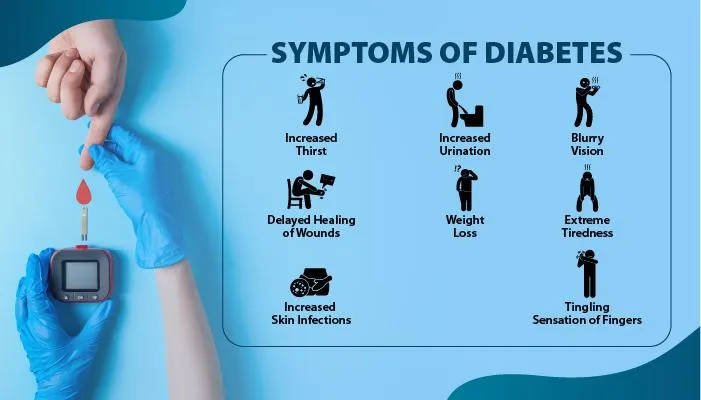
- Increased Thirst (Polydipsia): Dehydration resulting from frequent urination can lead to increased thirst.
- Extreme Hunger (Polyphagia): Despite eating regularly, individuals with diabetes may feel constantly hungry due to their body’s inability to effectively use glucose for energy.
- Unexplained Weight Loss: Type 1 diabetes often presents with unexplained weight loss, despite increased appetite, as the body breaks down muscle and fat for energy when it cannot use glucose properly.
- Fatigue: Feeling tired and lethargic is common in diabetes, especially when the body’s cells are deprived of glucose for energy.
- Blurred Vision: High blood sugar levels can cause fluid to be pulled from the lenses of the eyes, affecting their ability to focus properly.
- Slow Healing of Wounds: Diabetes can impair the body’s ability to heal, leading to slow healing of cuts, bruises, and infections.
- Frequent Infections: High blood sugar levels can weaken the immune system, making individuals with diabetes more susceptible to infections, especially in the skin, gums, urinary tract, and vagina.
- Tingling or Numbness in Hands or Feet (Neuropathy): Diabetes can damage nerves, leading to tingling, numbness, or pain in the hands, feet, or other parts of the body.
- Dry, Itchy Skin: Poor circulation and nerve damage caused by diabetes can lead to dry, itchy skin, particularly on the legs and feet.
It’s important to note that some individuals with diabetes may not experience noticeable symptoms, especially in the early stages of the disease. Additionally, the symptoms of Type 1 diabetes can develop rapidly, while those of Type 2 diabetes may develop more gradually and may be mistaken for other health issues. If you experience any of these symptoms or have concerns about diabetes, it’s crucial to consult a healthcare professional for proper evaluation and diagnosis. Early detection and management of diabetes can help prevent complications and improve overall health outcomes.
How to Help Someone with Diabetes
Supporting someone with diabetes involves a combination of practical assistance, emotional support, and encouragement. Here are some specific ways to help someone with diabetes:
- Encourage and Assist with Healthy Eating: Offer to plan and prepare balanced meals together, focusing on foods that help regulate blood sugar levels, such as whole grains, lean proteins, fruits, and vegetables. Be mindful of portion sizes and avoid sugary or highly processed foods.
- Promote Physical Activity: Encourage regular exercise and participate in physical activities together, such as walking, biking, or dancing. Physical activity helps improve insulin sensitivity and can aid in managing blood sugar levels.
- Support Medication Adherence: Help them stay on track with their medication regimen, including insulin injections or oral medications. Remind them to take their medications as prescribed and assist with refilling prescriptions when needed.
- Learn to Recognise and Respond to Hypoglycaemia and Hyperglycaemia: Educate yourself about the signs and symptoms of low blood sugar (hypoglycaemia) and high blood sugar (hyperglycaemia), and know how to respond appropriately. This may involve providing fast-acting carbohydrates for hypoglycaemia or helping them seek medical attention for hyperglycaemia.
- Be Understanding and Non-Judgmental: Living with diabetes can be challenging, and individuals may experience feelings of frustration, guilt, or stress. Be supportive and understanding, and avoid making judgmental comments about their lifestyle choices or blood sugar levels.
- Offer Emotional Support: Be there to listen and provide emotional support when needed. Offer encouragement and help them stay positive, especially during difficult times or when managing diabetes-related stress.
- Attend Medical Appointments Together: Offer to accompany them to medical appointments, if possible, and be an advocate for their healthcare needs. Take notes during appointments, ask questions, and ensure that they understand their healthcare provider’s recommendations.
- Educate Yourself About Their Specific Type of Diabetes: Different types of diabetes require different management strategies. Learn about their specific type of diabetes and any unique considerations or challenges they may face.
- Create a Supportive Environment: Help create a supportive environment at home and in social settings by promoting healthy habits and making accommodations when necessary. This may include keeping healthy snacks on hand, being mindful of meal timing, and accommodating physical activity into daily routines.
- Be Prepared for Emergencies: Familiarise yourself with emergency procedures for severe hypoglycaemia or other diabetes-related emergencies, including how to administer glucagon if needed.
By offering practical assistance, emotional support, and understanding, you can play a significant role in helping someone with diabetes effectively manage their condition and improve their overall quality of life.
Do you Really Know Diabetes: Our Courses:
On any of our first aid courses you will learn how to help someone who has a diabetes condition.
Our Emergency and First Aid at Work courses are for those working in an office, factory, warehouse, manufacturing or on a building site. These courses will set you up to know exactly what to do in an emergency. Completing our courses will help you understand the hazards and risks in your workplace to therefore prevent accidents.
Apprentices or staff who are unlikely to be left alone with children, and lunchtime supervisors are all candidates for our Emergency Paediatric First Aid Training. Our one-day course includes roles and responsibilities of a first aider, first aid kits, accident reporting, reasons of a life-threatening condition, CPR, defibrillator, causes of unconsciousness and recovery position, choking, bleeding, burns, and minor injuries.
Our Paediatric First Aid Training 2-day course includes all elements of the one-day first course including; broken bones, spinal injuries, head injuries, slings, sprains and strains, diabetes, febrile convulsions, hypothermia, hyperthermia, epilepsy, poisons, eye injuries, allergies and anaphylaxis, and asthma.
This course is ideal for those working alone with children, whether you are a Teacher or Teaching Assistant working in the Early Years or a childminder. Our Paediatric courses are fully accredited. We have open courses running at our Brownhills Centre or we can come to your setting.
Our courses provide you with the peace of mind that you’ll know what to do in the event of an emergency, such as illnesses like anaphylactic shock. Furthermore, getting first aid training will give you the skill set of knowing exactly what to do if your child, friend, or work colleague suffers from an injury or life threatening condition. Never put yourself in a situation where you’re thinking, “What if I knew what to do?” Get First Aid Trained Today! Do you really know diabetes
Call us on 01543 453338 or email us on info@hmbtrainingservices.co.uk



